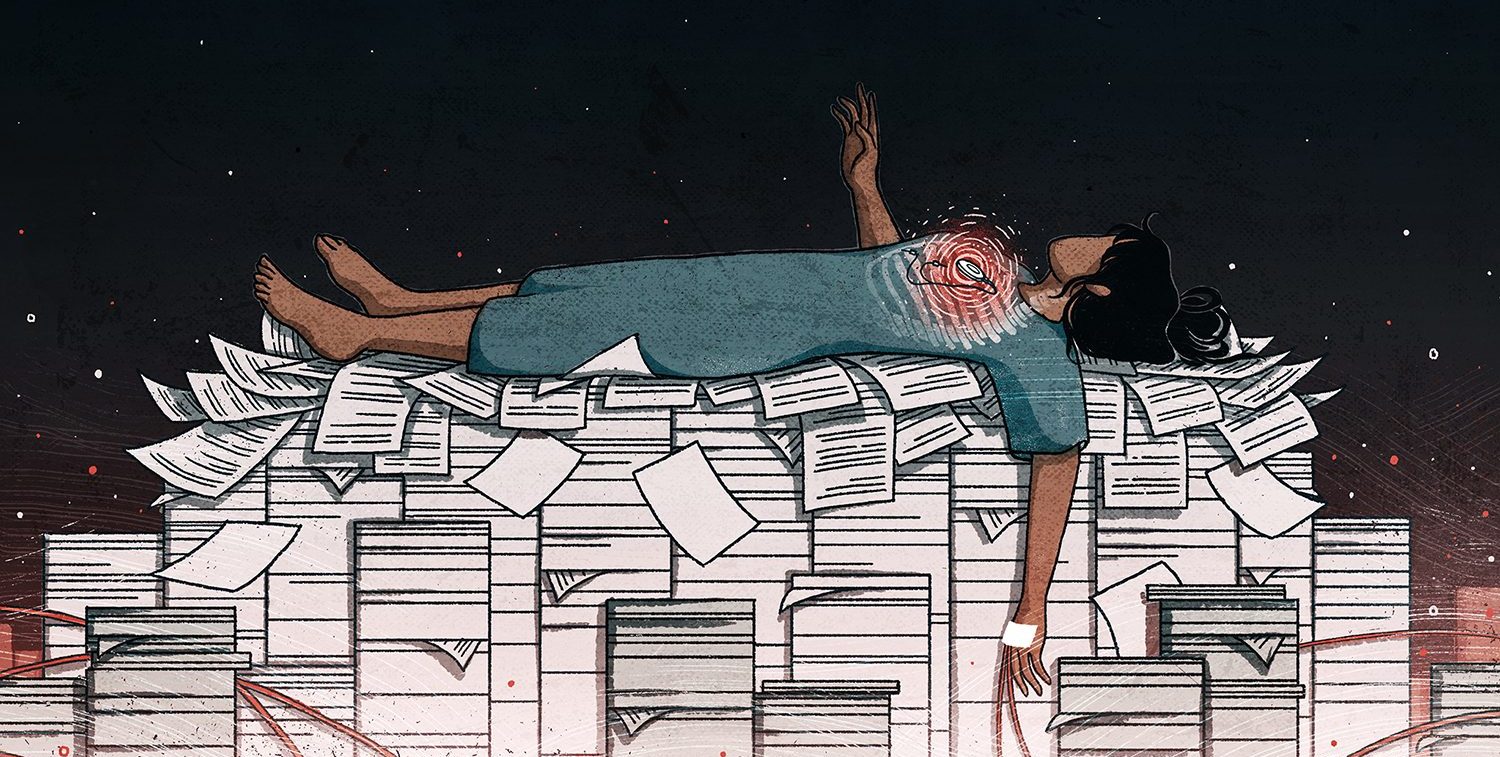
Senior doctors, consumer groups and transparency campaigners are urging the European Commission to force the manufacturers of high-risk medical devices to make public all the evidence they hold on the safety of their products.
The calls come just days after the International Consortium of Investigative Journalists and its media partners published the results of their year-long investigation into the medical device industry, known as the Implant Files.
A new law for medical device regulation in the European Union was passed last year, and comes into effect from 2020. It sets data transparency as one of its main goals, but the Commission – which has been the subject of intense lobbying from the device industry – has told ICIJ it plans to withhold detailed information in order to protect manufacturers’ commercial secrets and to avoid scaring the public.
Commission officials are shortly expected to announce what information manufacturers must share with doctors, patients and the public concerning the tests that were carried out on their product before they were certified as safe for use in hospitals across Europe. Officials will also make clear whether manufacturers’ files on device malfunctions and patient injuries – know as “incident reports” – will be made public.
“Transparency… should only be restricted when it affects the privacy of patients and individuals,” said the Spanish General Council of Medical Colleges in a statement in response to the Implant Files. “Existing data should be made public by default, and be accessible and usable on the Internet.”
Professor Terence Stephenson, chair of the United Kingdom’s General Medical Council, who carried out a critical review of medical device regulation in the U.K. four years ago, said: “These data sets should be publicly available in a way that is unbiased and comprehensible.”
In his 2014 review, Stephenson highlighted the link between public data and public health, arguing that publishing injury and malfunction reports would “significantly improve the safety of devices by empowering patients and healthcare professionals and increasing scrutiny on industry and regulators.”
It simply isn’t right or fair to have anything less than full transparency when it comes to the devices that are being used in healthcare.
In Sweden, Dr. Pia Caduff-Janosa, deputy director and chief medical officer of the Uppsala Monitoring Centre, said: “The same stringent regulatory principles for medicines should also apply for medical devices. But no regulatory process can be good enough without full transparency and open communication.”
It was a view echoed in France by Anne Chailleu, deputy president of Formindep, an organisation that campaigns for independent medical information for patients. “Access to all existing data, along with the possibility to audit and analyze them independently from the manufacturer or the payer is key to protect the patients and citizens interests.”
Dr. Till Bruckner, founder of TranspariMED, a global initiative working to end evidence distortion in medicine, said: “Why do companies have to make public the evidence they hold on heart drugs, but not on pacemakers? This is absurd. Doctors and patients need access to the full evidence on all drugs, devices and treatments. The new EU regulation for medical devices will fail to deliver on this basic transparency principle.”
In the U.K., Professors Michael Griffin, President of the Royal College of Surgeons of Edinburgh, and Carrie MacEwen, Chair of the Academy of Medical Royal Colleges, argued that withholding detailed data on the safety of devices jeopardised patients’ ability to give informed consent to their doctors.
“It is impossible for a patient to give informed consent to experimental treatment technologies, when the full short- and long-term consequences are not fully known,” Griffin said.
MacEwen added: “It simply isn’t right or fair to have anything less than full transparency when it comes to the devices that are being used in healthcare. It’s also vital that patients are monitored after any device is fitted to ensure it is both effective and safe in the same way as patients are monitored for any adverse drug reactions.”
Monique Goyens, director general of European consumer group BEUC and a long-standing campaigner for better medical device safety, said: “Information such as when patients have been harmed … should be available to allow public scrutiny of a particular device. Patients must have transparent and timely information, and be able to rely on the fact there is real and strong market surveillance, to avoid future health scandals.”
Reporters fight for medical device knowledge
Calls for data transparency come as ICIJ media partners across Europe continue to battle for more knowledge about medical devices using freedom of information (FOI) laws.
On Dec. 18, documentary-makers from ICIJ’s Dutch TV partner Avotros will attend a hearing at the offices of their national regulator concerning an FOI claim as part of their long-running efforts to obtain information about controversial medical devices from their national regulator.
Journalists are using freedom of information laws to try and discover what, if anything, Dutch regulators were told before a small trial of Nanostim – an untested, next-generation pacemaker – was started in patients in the Netherlands, Germany and the Czech Republic.
Traditional pacemakers, which are sited just beneath the skin, send impulses to the heart through leads. But the much smaller Nanostim was designed to be implanted directly into the heart, and could therefore operate without leads – a common cause of complication in other pacing devices.
In 2013, Nanostim received safety approval, based on the results of the small trial, which showed the product had worked well in 33 humans for three months.
Three years later, however, the manufacturer, U.S. firm St. Jude Medical Inc. (now part of Abbott Laboratories), halted use of the device when it learned of an alarming number of battery failures.
Experts have since questioned whether the first trial in humans had provided sufficient evidence to justify safety approval for a pioneering new device such as Nanostim. The product was implanted into more than 1,400 patients before its use was stopped.
In European law, Manufacturers must give details of any medical device trial to the national regulator before a study can start. Journalists from Avotros want to discover what the Dutch regulator was told about the Nanostim trial.
The regulator set up a hearing after Avrotros and Trouw objected to a decision to redact certain information from documents previously provided to the journalists. Lawyers from Abbott Laboratories are also invited for that hearing. The company claims that any disclosure would be a breach of confidence.
A recent study by another Dutch regulator found that 38 percent of trials were carried out in the Netherlands without proper notification to the local regulator.
Meanwhile, in France the national regulator this week refused to give journalists from Le Monde newspaper, an ICIJ media partner, information concerning medical devices. The regulator cited new European trade secret laws as the justification for its refusal to release copies of the documents requested. It is the first time these trade secret laws have been used in France to block a request made by a journalist. Le Monde is contesting the decision.
Correction, Dec. 4: An earlier version of this article incorrectly stated ICIJ’s Dutch media partners Avotros had a court hearing last week regarding an FOI claim, and that Abbott Laboratories had joined the case. The hearing is before the national regulator, not the courts. The hearing is scheduled for Dec. 18. Lawyers from Abbott Laboratories have been invited to join.