The U.S. Food and Drug Administration said Monday that it will enact the “most significant modernization” in a generation of how the agency clears most medical devices for sale.
The agency is focusing on a heavily used pathway for approval based not on human testing but on similarity to older approved devices. The news that the FDA is considering revamping the process comes a day after ICIJ and 58 media partners published findings from the Implant Files, a global investigation of the medical device industry and its governmental regulators that included detailed descriptions of problems that had arisen from that approval process.
FDA Commissioner Scott Gottlieb, announcing the changes along with the agency’s device chief Jeffrey Shuren, highlighted their historical significance. He also acknowledged that the substantial equivalence test, known as 510(k), has allowed new devices to be approved for sale based on their similarity to devices approved decades ago.
“We believe firmly in the merits of the 510(k) process,” said Gottlieb. “But we also believe that framework needs to be modernized to reflect advances in technology, safety and the capabilities of a new generation of medical devices. In short, we believe that it’s time to fundamentally modernize an approach first adopted in 1976.”
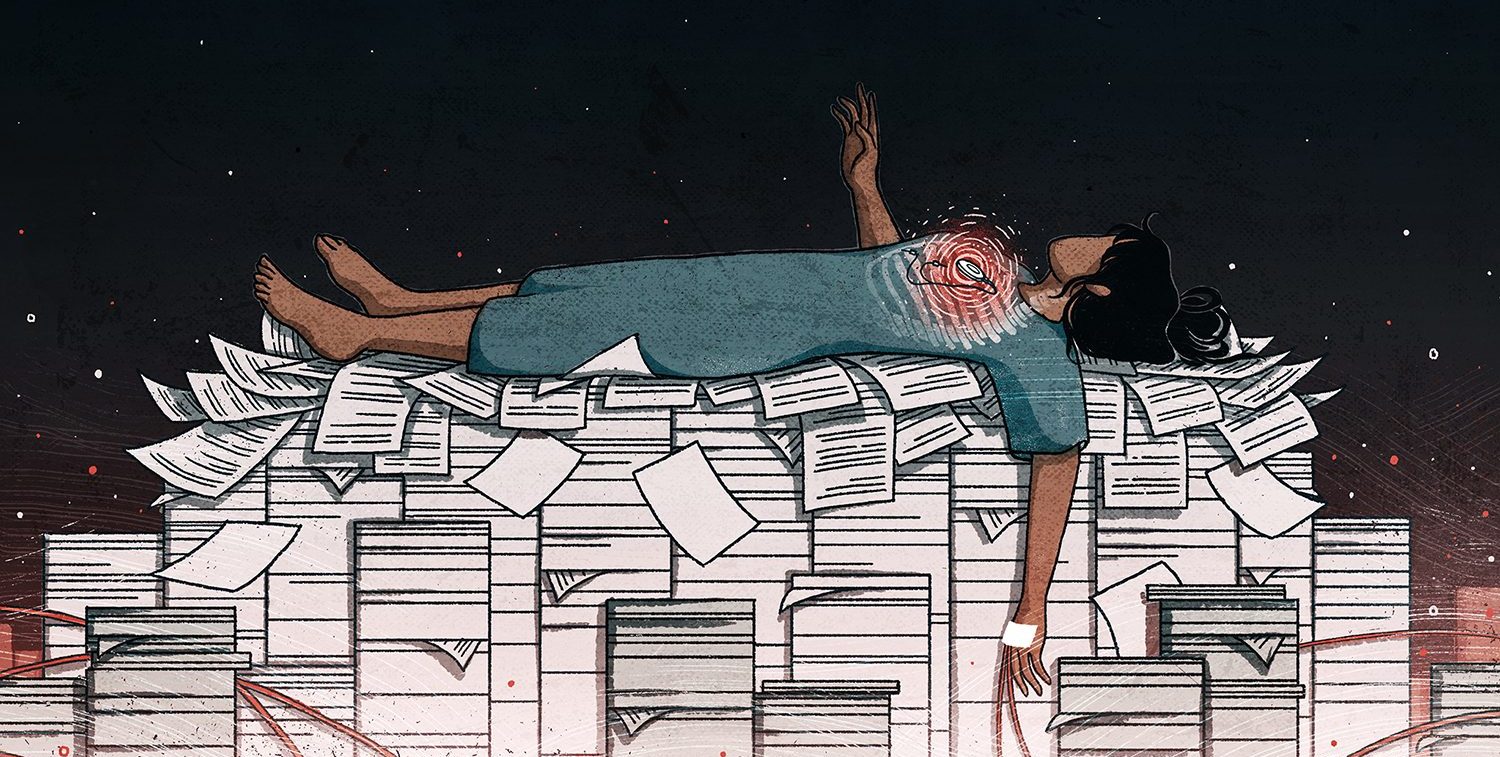
This substantial equivalence path to approval is just one of many areas of weak device oversight highlighted in a 12-month investigation by ICIJ and its global reporting partners. The investigation found that governments around the world hold even highly complex implants to a lower safety testing standard than most new drugs.
It also found that flawed devices can linger on the market for years as injuries mount. Apart from weak approvals, the investigation also found significant problems in the way safety problems are communicated by national regulators, device companies and doctors around the world. Device companies sometimes pull implants in some countries while continuing to sell them in others, the Implant Files investigation found. More than 200 patients with implanted medical devices told ICIJ and its partners that they were not warned of crucial risks of their devices or notified of recalls or safety alerts.
The FDA is generally considered to have the world’s most robust — if still imperfect — oversight of medical devices, resulting in device regulators in countries across the globe often following its lead on which devices to sell domestically. “Products that are harmful can spread across the world very quickly,” according to Carl Heneghan, a U.K.-based epidemiologist and director of Oxford University’s Centre for Evidence-Based Medicine. The 510(k) route has been widely identified as the weakest aspect of the FDA’s device approval standards and is alleged to have contributed to hundreds of thousands of defective devices being implanted in patients around the world.
Some of the largest global device controversies in recent years were rooted in that process. A variety of metal-on-metal hip implants, associated with a range of severe complications, were cleared through FDA’s substantial equivalence route, only to be removed from the global market years later amid grave safety concerns.
Sometimes after a chain of equivalence-based approvals, a new iteration of a device scarcely resembles the original version. Research published by ICIJ partner BMJ, traced the family tree of 61 surgical mesh products to two original devices approved in 1985 and 1996. None had completed clinical trials to win approval.
The FDA’s announcement addressed the distance in years between some devices from their predicates. Focusing on companies that clear new devices based on products more than a decade old, the proposal calls for encouraging companies to use comparisons to more recently approved devices when seeking approval through the 510(k) process. The agency also noted separate changes the agency has made to the 510(k) pathway in recent years.
Among the most concrete steps outlined in the announcement is FDA’s plan to create a website listing all devices approved based on a previous version more than a decade old. “It looks like what they’re trying to do is shame companies into using newer devices when they seek clearance in this pathway,” Dr. Michael Carome, the director of Public Citizen’s Health Research Group, told ICIJ.
Industry groups argue that the 510(k) route is necessary because devices are constantly being improved incrementally. From a practical standpoint, human testing doesn’t make sense in such cases, according to the industry.
AdvaMed, the main American trade association for medical device makers said that, in some cases, it is proper and safe to use older versions of a device to approve new ones. The group said that the FDA’s concerns regarding using older devices as predicates only applies to a minority of devices that have no demonstrated safety concerns. “The proposed 10-year cut off criteria could prove arbitrary as older predicates can offer extensive data about their performance, which helps sponsors introduce newer, safer devices,” the group said in a statement.
Despite the strong wording of the agency’s statement, Carome of Public Citizen said he doubts it will herald historic change to the FDA’s troubled approval process. As worded, the proposal does not call for any increase in clinical testing to win approval through this pathway, Carome noted. “The 510(k) process remains a fundamentally flawed approach to medical device oversight.”