The New Orleans sales conference of medical-device maker DePuy Orthopaedics Inc. was rocking. The sound system blasted “Takin’ Share of Business!” — a play on the ‘70s hit tune — as top company executives boogied in Mardi Gras-style costumes through a hall full of sales personnel.
And why not? DePuy, a unit of healthcare giant Johnson & Johnson, was dominating one of the hottest products in the medical device industry: “metal-on-metal” replacement hips, touted as more durable than traditional varieties that use plastic and other materials.
Leading the way was DePuy’s cornerstone brand, Pinnacle, which had helped the company capture more than half of that market.
On came the evening’s main attraction: Thomas Schmalzried, a Pinnacle developer and renowned orthopedic surgeon, with a 34-page resume of honors, board memberships and publications.
This evening, captured in an early 2008 video later uploaded to Youtube and featured in a 2017 exposé by KABC-TV, Los Angeles, he sounded more pitchman than physician.
“Your billion-dollar baby — Pinnacle with high-performance bearings; you are the market leader,” Schmalzried said.
“But did you know you can sell even more?” he added. “Did you know that the first billion is the hardest? Billion here, billion there. Pretty soon it adds up to some real money.”
“Anyone here want to go for two? I’m gonna say that again. Does anyone here want to go for two?”
The sales force crowd whooped and cheered.
“That’s what I’m talkin’ about!,” the surgeon said.
The sales meeting in New Orleans would be the high-water mark for metal-on-metal hips. Propelled by an aggressive marketing campaign and, investigations later found, kickbacks and bribes to surgeons, the Pinnacle hip system and a sister product that Schmalzried also helped design, the ASR XL, sold like crazy, helping to drive DePuy’s overall 2008 sales to $5 billion.
But, like the vast majority of devices sold in the United States and around the world, neither Pinnacle nor ASR XL had been tested in a human being before coming to market.
ASR XL and ASR, a related product, were recalled in several countries, including in the United States in 2010, and Pinnacle was pulled from the market amid a flurry of lawsuits as the metal-on-metal market began to collapse. Hipmakers Zimmer Biomet, Smith & Nephew, Wright Medical, and Stryker all removed their metal-on-metal hip devices or components from the market amid a welter of alarming reports globally about poisoning from tiny metal ions that turned surrounding tissue to a liquified black sludge.
The hip manufacturers say they fully support their products and are committed to safety.
A spokesman for Johnson & Johnson, said: “We stand behind the safety of our devices, which have benefited millions of patients who continue to find relief from the debilitating conditions that necessitated them to undergo surgery. We meet, and strive to exceed, required regulatory standards, and our devices … are subject to careful reviews by multiple regulatory bodies around the world. Once made available for use, we continue to analyze information such as clinical data and adverse event reports to track its performance.”
‘Almost a perfect storm’
Diana Zuckerman, president of the National Center for Health Research, a think tank based in Washington, D.C., said the metal-on-metal disaster was emblematic of deep cultural and structural flaws in the device regulatory regime that are the focus of the Implant Files, a year-long global investigative led by the International Consortium of Investigative Reporters. Legal loopholes and too-close ties between regulators and industry, combined with years of attacks on the very idea of regulation by industry and politicians, allowed dangerous devices to breeze onto the market and linger for years.
“It was almost a perfect storm,” Zuckerman said.
The arc of the metal-on-metal hip business helps to illustrate the trajectory of the medical devices industry writ large — from the domain of physician-tinkerers and small entrepreneurs to transnational corporations that are a pillar of the $7 trillion global healthcare industry and powerful players in Washington, Brussels and other capitals around the world. A fund of leading medical device stocks returned a sparkling 125 percent in the last five years as of Nov. 14 compared to 52 percent for the broader economy reflected in the Standard & Poor’s 500.
Nearly 1 million people worldwide are implanted with transvenous heart pacemakers each year, the U.S. Food & Drug Administration reports; more than 1.6 million women worldwide got cosmetic breast implants in 2017, according to the International Society of Aesthetic Plastic Surgery.
And the industry’s fastest growth now comes from developing markets, where wealth is rising but regulation is weak.
Medical device companies have achieved remarkable successes over the years: intraocular lenses to fix cataracts, pacemakers that regulate heart rhythm, hip and knee replacements that restore mobility to millions of people, and more.
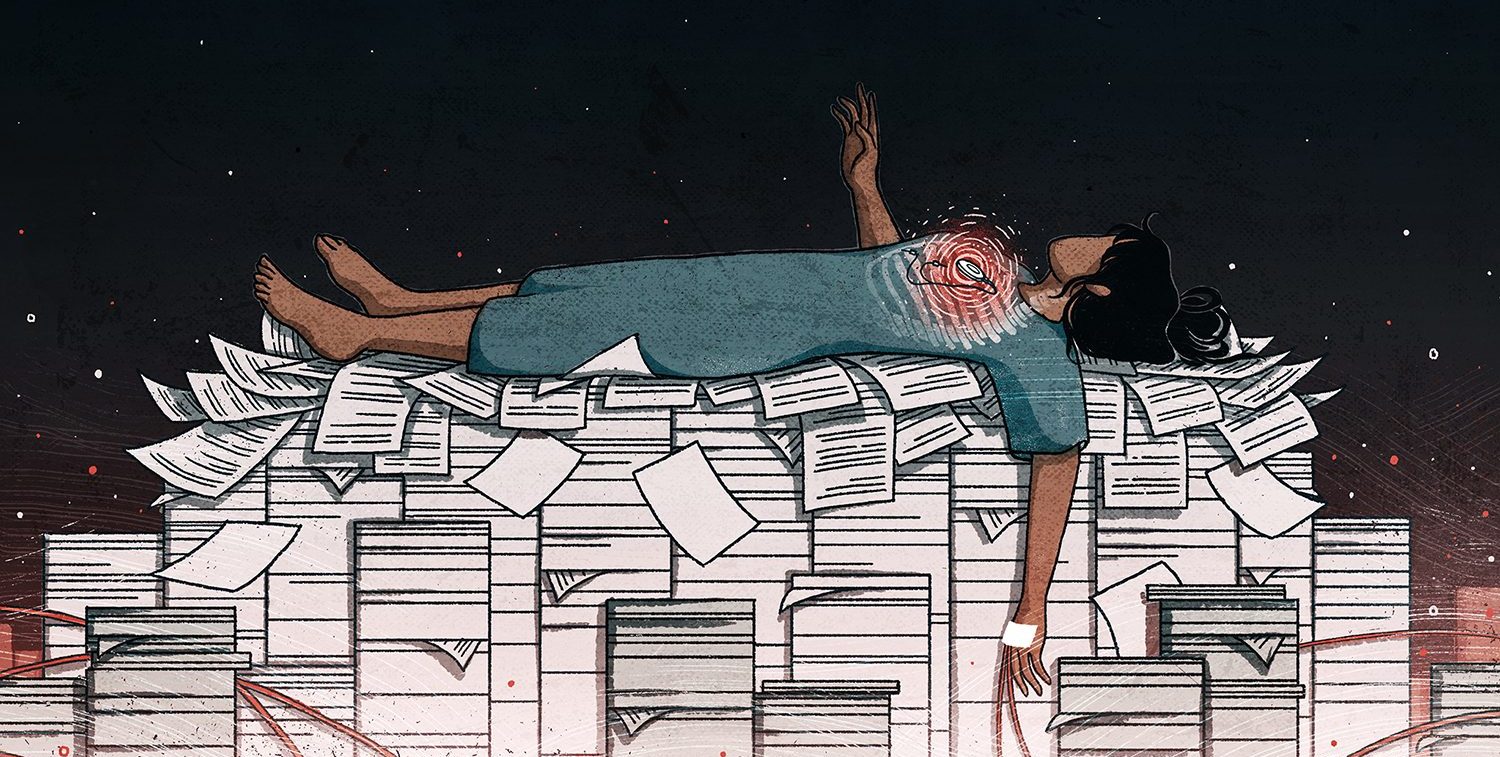
But the industry is also saddled with a long history of rushing flawed implantable products to market that can injure, maim and kill. Devices are often approved based on scant clinical evidence of safety or effectiveness — sometimes supported by research paid for by the industry itself. They are then aggressively marketed to doctors and hospitals in ways that push — or break — legal and ethical barriers.

Rise of the device-industrial complex
The use of implanted devices to improve health dates to bronze catheters used in Roman times and before. But the medical breakthroughs of World War II and the prosperous decades that followed ushered in a healthcare revolution that would vastly expand what was medically possible.
The creation of U.S. Medicare in 1965 and the rise of public and private insurance markets in the United States and Europe provided a way to pay for the innovations. German healthcare spending zoomed to 10.6 percent of gross domestic product by 2000. U.S. healthcare exploded. In 1950, healthcare cost $12.7 billion nationally and made up 4.5 percent of U.S. GDP. By the end of 2016, it was 17.9 percent, or $3.3 trillion, according to the Centers for Medicare & Medicaid Services.
That’s $10,348 a year for every man, woman and child in the U.S.
The pharmaceutical industry was an early beneficiary of increased spending. Bayer AG, Merck & Co., Pfizer Inc., Eli Lilly & Co. and their predecessors — brought to market an armada of new drugs: antibacterials to attack tuberculosis, dysentery, scarlet fever, whooping cough and pneumonia; antihypertensives to take on heart disease; statins to lower cholesterol; contraceptives to manage family planning. The success in 1954 of the Salk polio vaccine trials, which led to prevention of a dreaded childhood disease, triggered a national celebration and cemented public faith in doctors, medicine and the scientific method.
Death rates everywhere plummeted. Life expectancy soared.
In the shadows of Big Pharma, a second arm of this new medical-industrial complex would rise separately and less visibly.
Medical devices, including manufactured products implanted in the human body, would bring to market additional breakthroughs that saved and dramatically improved lives. Filters to catch blood clots on their way to the heart; stents to hold arteries open; mesh to patch holes in abdominal walls to treat hernias were among the simpler, early products invented by physician-tinkerers and entrepreneurs.
John Charnley, a former British Army surgeon who had treated soldiers in Dunkirk during the historic evacuation of 1940, labored in obscurity for years to build a workable artificial hip. In his search for the right material to form the hip socket, he once injected an experimental resin into his own thigh — and became gravely ill. Eventually his metal-on-polyethylene “total hip arthroplasty [replacement]” system, announced in 1960, would be hailed as one of the great medical achievements of the 20th century, bringing relief to millions of patients globally and a knighthood for Charnley in 1977. It would also launch a fiercely competitive new industry.
Over time, devices became even more ambitious and ever more complex: deep-brain stimulators, spine implants with biologically active bone-growth stimulators, cloud-enabled pacemakers, brain-fluid shunts, hormonal implants, vagus nerve stimulators to treat epilepsy and depression and more.
Medtronic PLC, founded as a medical device repair shop in 1949 in suburban Minneapolis, developed the first wearable pacemaker in 1957 and would become a Wall Street darling with an acquisition spree in the following decades. Johnson & Johnson, a surgical-dressings maker founded in the late 19th century, went public during World War II and grew into a pharmaceutical and device giant, boosted by its 1998 purchase of DePuy.
Pharma is big: about $1.1 trillion in global revenue. The device business is also big: about $400 billion. It is also complex, producing more than 500,000 different products compared with about 20,000 different medicines. And it is ubiquitous: a 2002 study found that one in 10 Americans had been implanted with a medical device.
But there’s one big difference between the two. Drugs are tested in human beings before coming to market. In the overwhelming number of cases, medical devices are not.
Most, instead, are approved on the claim that they are similar enough to another version, or versions, of the same or similar product as to not require new human trials. Even when human trials are required, the standard is lower: drugs are usually subjected to multiple trials, devices usually just one.
The generally lower testing standards for devices have contributed to a string of recalls, disasters and scandals of a kind once common in the drug industry that continue to plague devices to this day. In the last dozen years, the industry has experienced critical failures with metal-on-metal hips, transvaginal mesh, lightly tested heart devices, among others.
All problematic versions are now gone from the market or heavily restricted.
Heart valves and toasters: a regulatory blind spot
Pharmaceuticals are more closely watched because regulation typically comes in response to scandal — and drug scandals came early and often in U.S. and European history.
It took an uproar over Elixir Sulfanilamide, a strep-throat medication containing antifreeze chemicals that killed more than 100 children and adults, to spur the U.S. Congress to pass the Food, Drug and Cosmetic Act of 1938. The law empowered the U.S. Food and Drug Administration, which had primarily been concerned with food hygiene, to regulate drug safety. The scandal of the 1950s around thalidomide — a nausea drug given to pregnant women that produced horrid birth defects — caused Congress in 1962 to further strengthen drug safety standards.
Medical devices, meanwhile, went virtually unregulated in the United States, as the industry grew into an economic and lobbying force. In 1971, the pharmaceutical company A.H. Robins began marketing the Dalkon Shield, an intrauterine contraceptive device that would be used by more than 2.5 million women. Before long, the device was traced to ghastly infections, pregnancy-associated complications, loss of fertility, hundreds of thousands of legal claims and public furor.
Congress passed the Medical Device Amendments of 1976 (amending the 1938 law), finally empowering the FDA to oversee approval of medical devices but leaving loopholes. For one thing, devices are classified according to perceived risk, allowing the agency wide discretion in testing standards. Plus, the law allowed any device already on the market, even high-risk ones, to be “grandfathered” in without testing. Another provision, known as 510(k), allowed new devices onto the market if they were “substantially equivalent” to a product already on the market, even if the earlier product was itself untested and even if it later fails to the point of recall.
Of all the implanted devices recalled in the United States from 2008 to 2017, 80 percent had been approved based on substantial equivalence, ICIJ found.
As regulatory standards eroded, the 510(k) exception became the rule. Now, about 97 percent of reviewed devices go through 510(k) or some other faster route.
Over the years the FDA’s relative clout has grown weaker as Congress has passed laws making the agency dependent on manufacturers’ fees for part of its revenue, allowing private parties to approve changes to risky devices and more.
And while the FDA has struggled to maintain its autonomy from business, in Europe, medical device approval is a business.
The job is mostly left to private companies paid by device-makers. This privatized system has led to a string of products barred in the United States that made their way into Europe, only to wreak havoc. Among these: PleuraSeal, a lung sealant that leaked; Trilucent breast implants, approved without human testing, that proved toxic; RoboDoc, a robotic surgical device that caused tendon rupture and nerve damage.
The model dates to the 1980s, when nations of the nascent European Union moved to standardize regulation of consumer and industrial goods by designating so-called “Notified Bodies” to inspect and approve products by issuing a seal of approval. With most exempt from public records laws and viewing manufacturers as “clients,” the notified bodies are nonetheless responsible for certifying the safety of everything from cars to toasters to breast implants.
The European device industry openly touts the speed at which Europe approves devices as a key advantage over the United States to device makers. Wall Street also views Europe’s system favorably.
Many developing countries with even weaker regulation defer to approvals issued in Europe and the United States, although some may be forced to change.
India is now moving to set up its own system to regulate devices after a health ministry panel found that metal-on-metal hips approved without testing in Europe and the United States constituted “serious medical negligence” by Johnson & Johnson’s DePuy unit.
The dramatic rise and fall of metal-on-metal hips exposed the flaws of both the U.S. and European systems.
The metal-on-metal hip disaster
Metal-on-metal devices had been used on a limited scale since the 1950s but were never adopted widely because of safety and other concerns. What was believed to be a breakthrough arrived in 1997 when an orthopedist in Birmingham, England, announced a less invasive technique that used metal for both hip and socket.
The new hip gained swift approval in Europe. The U.K.’s BSI Group, the private “notified body” authorized to vet products, classified it according to an E.U. directive at the time as medium risk, requiring only lab work and clinical literature reviews — no human testing.
In a statement, BSI said the device was “withdrawn from the market some time ago. At the time of assessment, the products met all the requirements of the Directives.” BSI added that it “places paramount importance on patient safety” and “to ensure our independent conformity assessments are robust, BSI continually invests in clinical and technical specialists with considerable experience and expertise across an array of medical device industry sectors.” It noted that metal-on-metal hips are now in a higher risk category, requiring “a product specific evaluation by the notified body.”
Sales of the new hip boomed. Competing hip makers flooded regulators with their own metal-on-metal models.
In the U.S., both the Pinnacle hip replacement system and the ASR XL, which had important technical differences, were cleared under the FDA’s 510(k) “substantial equivalence” standard.
In August 2000, DePuy won clearance for a metal-on-metal hip product called Ultima based on an application that claimed it was similar to four earlier hips — including a non-DePuy hip that had undergone extensive trials and two others that were abandoned amid performance concerns. There was a clinical trial for Ultima.
Pinnacle was cleared a few months later based on its similarity to Ultima.
ASR XL’s 510(k) application had its own quirks. Approval for its various parts could be traced back decades through 95 different devices, including several discontinued ones, according to a researched opinion piece in the New England Journal of Medicine. Clearance for metal-on-metal parts was based on three prostheses used before 1976 that had been discontinued for poor performance. A peer-reviewed medical journal article said those older components were abandoned amid high failure rates, reaction to metal debris and concerns about metal ions. Nonetheless, the ASR XL was cleared by the FDA in 2005.
The J&J spokesman said the FDA decided only after “careful consideration” to clear metal-on-metal hips through the 510(k) pathway, which can involve extensive clinical and other trials. He said that a predecessor to the Ultima, known as Metasul, was introduced in Europe in 1988 and later underwent human testing in the U.S. on par with that required for the FDA’s most rigorous pathway. He said that there was extensive medical literature reporting on its clinical success over time. Pinnacle itself had been through two clinical trials of its safety and effectiveness after it had come to market and had “demonstrated excellent results,” he said, and multiple published, peer-reviewed articles had shown Pinnacle metal-on-metal “has been safe and effective in those patient populations.” He added that the FDA had required its most rigorous pathway and multiple clinical trials for a related metal-on-metal hip procedure, known as resurfacing.
The spokesman said devices were removed from the market for many reasons, and that “older designs were inevitably phased out as designs evolve and medical and scientific knowledge advances.” He said the predicate devices no longer on the market didn’t form the “essential basis” for the FDA’s approval of Ultima but were included to demonstrate that metal-on-metal hip replacements were in use prior to the 1976 Medical Device Amendments. He said FDA required every manufacturer of newer metal-on-metal devices, including J&J, to submit clinical evidence of safety and effectiveness of the manufacturer’s own initial metal-on-metal total hip replacement, and there’s no reason to believe FDA ignored the data manufacturers submitted and contemporary knowledge in evaluating the devices.
The FDA would eventually clear 190 different metal-on-metal total hip-replacement systems for five different manufacturers, most through the 510(k) pathway.
Hip companies spent huge amounts on direct payments to surgeons through grants, fellowships, royalties and consulting deals. DePuy paid surgeons $184 million in royalty payments alone on Pinnacle-related designs, according to evidence presented in civil trials. Schmalzried, the hip developer and booster, received a percentage for devices sold, helped prepare DePuy sales material, and trained medical residents and occasionally other doctors in the use of the products. He earned $30 million in royalties from J&J/DePuy over less than two decades.
The J&J spokesman said the company “has rigorous compliance policies and procedures governing royalty arrangements. Collaboration with surgeons has been an integral part of the orthopaedics industry for many years, as the intellectual property for orthopaedic products, which forms the basis for any royalty payment, is often originated or owned by the physician. Importantly, royalties are not paid on any products implanted in patients by the royalty-earning surgeon, the surgeon’s partners, or at the surgeon’s hospital.”
Through a representative, Schmalzried declined to comment.
A U.S. Health and Human Services inspector general’s investigation would find that the hip and knee makers spent more than $800 million in consulting fees alone to surgeons. Sales and promotional practices would lead to federal kickback charges and settlements with major hip makers. Former New Jersey governor Chris Christie, as a U.S. attorney in the 2000s, would later allege: “Many orthopedic surgeons in this country made decisions predicated on how much money they could make — choosing which device to implant by going to the highest bidder.”
By May 2013, more than half a million Americans had received metal-on-metal hips.
Direct-to-consumer, or DTC, advertisements were a big reason. “98 percent of surgeons say their patients were exposed to DTC,” says an internal DePuy slide presentation. “99 percent say patients ask for a brand.”
In 2007, Biomet, now part of Zimmer Biomet Holdings Inc., of Warsaw, Indiana, enlisted Mary Lou Retton, the 1984 Olympic gymnastics champion, as spokeswoman for its M2a-Magnum product.

“The M2a-Magnum hip is a perfect 10 with me,” Retton says in full color ads picturing her, then 50 years old, playing soccer with her young children and smiling on a treadmill after undergoing replacement surgery on her left hip in 2005. She subsequently had her right hip replaced with the Biomet device in 2011.
In statement to ICIJ, Monica Kendrick, Zimmer Biomet’s Vice President, Corporate Communications said: “The safety of patients has always been, and continues to be, Zimmer Biomet’s top priority and it is our honor to be a leader in this industry for the past 90 years. We adhere to strict regulatory standards, and work closely with the FDA and all applicable regulatory agencies in each of our regions as part of our commitment to operating a first-rate quality management system across our global manufacturing network. Zimmer Biomet is focused on staying at the forefront of innovation and doing right by the millions of patients who rely on our products.”
If anything, metal-on-metal marketing was even more aggressive in Europe.
By early 2000, Johnson & Johnson executives learned that DePuy for years had routinely sent payments to a Greek distributor and an Isle of Man consulting firm, both owned by a Greek intermediary who paid off Greek surgeons. Ostensibly the payments were for “professional education,” but were later revealed by the U.S. Securities and Exchange Commission as cash bribes to use DePuy hips. J&J considered ending the relationship, court documents revealed, but instead bought the Greek distribution firm, continued the consulting deal with the Isle of Man company and kept the payments going.
Bribes to surgeons in Greece and elsewhere were common knowledge across the device industry, investigations would reveal. When rival Smith & Nephew PLC of the U.K. moved in 2002 to reduce payments to its own third-party distributor, the distributor protested in an email: “I absolutely need this fund to promote my sales with surgeons, at a time when competition offers substantially higher rates … In case it is not clear to you, please understand that I am paying cash incentives right after each surgery.”
“The matter you refer to relates to events more than ten years ago and do not reflect the values and practices of Smith & Nephew today”, a spokesman from the company told ICIJ. “We have very high expectations for the conduct of our employees at all levels of the company.”
Nearly a million people a year in the major Western economies, including more than 600,000 Europeans, were getting their hips replaced by the middle of the decade. One was British systems analyst Steve Allen. He said he began to develop hip arthritis in the early 2000s and first tried a technique less invasive than total hip replacement. When that went quickly wrong, his surgeon recommended Pinnacle, and Allen underwent total replacement in 2006. Soon he was swimming and walking again. “To be honest it was absolutely wonderful,” Allen, 70, says. “The pain went like that.”
A few years later, though, he began to notice an odd feeling, like “a little handbag” was buried in his hip. He started to walk with a hobble.
By this time, officials at the Australian National Joint Replacement Registry, the government-funded research arm of the Australian Orthopaedic Association, had begun to notice strangely high failure rates for ASR XL, forcing DePuy to issue a safety warning to surgeons in 2007. The warning suggested surgeons were implanting them incorrectly, not that the product was a problem.
But surgeons in different parts of the world were already talking among themselves about serious metal-on-metal problems. A 2008 internal email from a DePuy executive attending a Hip Society conference in Chicago reported, “Visually, the MoM cases looked alarming and disturbing. . . . The images for MoM reaction looked bad.” He added that the data and cases presented didn’t show MoM had caused the problems, “but 80 percent of attendees had seen this kind of tissue reaction.”
A DePuy hip-marketing executive who had introduced Schmalzried at that New Orleans sales conference the same year, replied: “Hang in there. We’ll manage through this.”
The metal-on-metal hip disappearance
Today, metal-on-metal hip replacements have virtually disappeared from the market. Health authorities recommend patients who still have them get checked every year or two — or as soon as they suspect they have hip-related health problems. Those with symptoms often need a new hip.
In 2010, DePuy announced a global recall of its entire ASR XL product line, as courthouses around the world were flooded with claims for product liability, personal injury and fraud.
I’m so angry and frustrated about this lack of explanation, and I believe that this is a baby that should not have come out in this world.– Jeong Sang Ho
In India, a health ministry panel recommended in January that each patient receive about $30,000 in compensation. The final amount has yet to jo confirmed.
The U.S. FDA in 2011 issued a bulletin, “Concerns about Metal-on-Metal Hip Implant Systems,” and would later reverse itself and finally require makers to produce clinical data to justify the use of metal-on-metal hips, as with pacemakers and other risky medical devices.
By 2014, J&J/DePuy, Smith & Nephew, and Zimmer Biomet had all settled criminal and civil charges with the U.S. Justice Department and U.S. Securities and Exchange Commission related to European bribery. Stryker settled SEC charges without admitting or denying wrongdoing.
“We operate in a regulated industry and the quality of our products for patients and caregivers is our top priority. We remain committed to working with our customers to make healthcare better while operating ethically and in compliance with all applicable laws and regulations,” a Stryker spokesperson told ICIJ.
More than 28,000 lawsuits would be filed in cases naming virtually all metal-on-metal hip makers. Mary Lou Retton, under the surname Retton-Kelly, sued Biomet, alleging its hip was defective, inadequately tested and caused excessive cobalt levels in her blood, “disfigurement” and other permanent injuries. The case is pending.
After a 2013 jury verdict in Los Angeles awarded $8.3 million to an ASR XL patient, DePuy announced a $2.5 billion fund to settle ASR XL claims; settlements later climbed to $4.4 billion.
And then Pinnacle verdicts started to roll in. After siding with J&J/DePuy in the first so-called bellwether case, federal juries in Texas began awarding staggering sums, including the $1 billion verdict in a December 2016, nearly all of its punitive. Some of the biggest judgements were later reduced or reversed.
Around the world, redress has been as uneven as regulation.
A South Korean patient, Jeong Sang Ho, who had a defective ASR XL replaced by a second one in 2010 before knowing about any recalls, received only about $620 from Johnson & Johnson’s Singapore unit through a Korean insurance adjuster. He is suing in a case pending in a U.S. federal court, though foreign plaintiffs can face additional legal hurdles.
“I never received any explanation of the risk of this device,” Jeong told ICIJ’s media partners. He said he has cobalt levels five times normal levels, lost his job as a result of fallout and now has trouble lifting an infant. “I’m so angry and frustrated about this lack of explanation, and I believe that this is a baby that should not have come out in this world.”
The J&J spokesman said, “It is the company’s practice to monitor the totality of the data from a variety of sources, including joint registries, published literature, company-sponsored clinical trials, internal complaints data and external clinical research reports. Our ongoing monitoring of clinical data for (Pinnacle) ULTAMET Metal-on-Metal has continued to show a track record of reducing pain and restoring mobility for patients suffering from chronic hip pain.”
He added that the company has “voluntarily compensated ASR patients by taking the unprecedented step of addressing the costs of recall-related medical care and associated out-of-pocket expenses and lost wages through the ASR Reimbursement Program. The Program is available to all patients globally, and participating in the program does not require patients to waive their legal rights to pursue a claim against the Company.”
Steve Allen, the British systems analyst, said doctors exploring his hip discomfort had found metal ions in his blood. He finally had the Pinnacle implant removed in 2014 and was told by his surgeon that “the damage was absolutely incredible.” He now has a hip made of metal-on-polyethylene and says he feels fine, but after all the surgeries, mobility remains a problem. Despite gym visits and physical therapy, “I walk as though I’d just landed after a life at sea.” He continues treatment with an orthopaedist.
Allen was among 312 claimants in a long trial that ended in May in England alleging that Pinnacle violated the country’s consumer protection laws and regulations.
The judge ruled in that trial that the Pinnacle hip was not defective and found against the plaintiffs. In her ruling, the judge said that despite the European and U.S. approvals, surgeons were “all aware” that Pinnacle devices did not undergo human testing, and “it was unknown how well they would perform in real life.” Plus, she wrote, the product’s “instructions for use” contained warnings about unknown risks of metal ion leakage.
The J&J spokesman noted that the U.K. judge said, among other things, that the Pinnacle was “a well-designed product with many positive engineering features.” The spokesman also said that the court found that “although a metal-on-metal product would, by its very nature, produce metal wear debris – which in turn might cause an adverse reaction in some patients – that was not in itself a defect” for the purposes of the country’s consumer protection laws.
The sweeping decision left little room for appeal and has dealt a potentially mortal blow to Pinnacle suits still pending in England and Wales.
Allen, who had attended several days of the trial, remains stunned. “I find it hard to let go of an injustice,” he says.
Contributors: Boyoung Lim and Spencer Woodman.