IMPACT
US government audit identifies ‘challenges’ in FDA’s monitoring of medical devices linked to patients
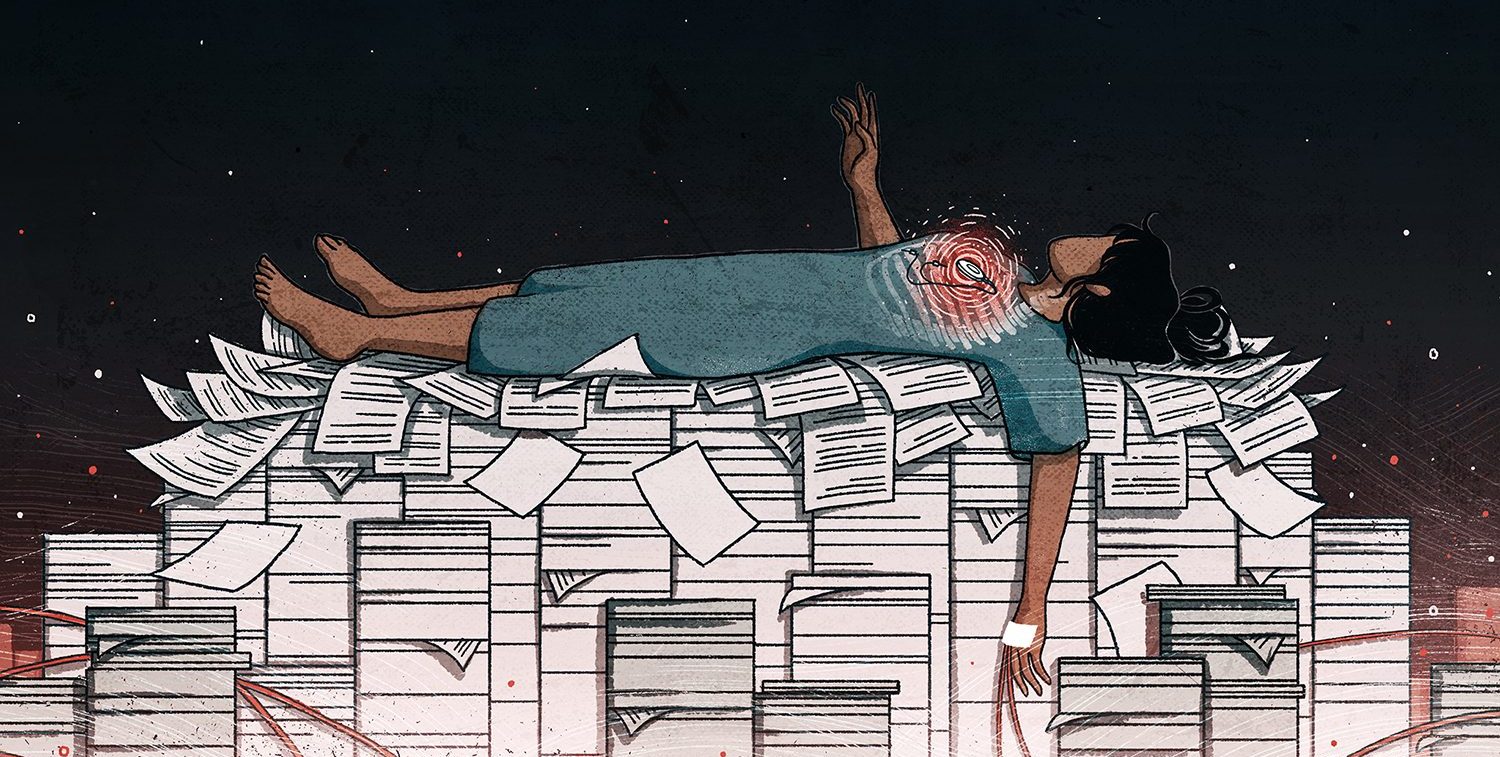
An oversight initiative meant to help officials detect medical device safety issues has faltered due to patchy recordkeeping by health care professionals.

A U.S. government audit found shortcomings in the Food and Drug Administration’s oversight of medical devices and cited the results of a data analysis by the International Consortium of Investigative Journalists of device-related injuries and deaths.
The audit report by the Government Accountability Office said that FDA officials were struggling to implement an “active” surveillance program mandated by law 12 years ago due to a lack of information that would allow them to identify devices used by patients and detect potential safety issues.
The program hinges on the effective use of so-called “unique device identifiers,” or UDIs, that help link products to patients using them. After taking nearly 10 years to ensure most types of medical devices have UDIs, the agency cannot fully rely on them to monitor the safety of products because health care providers and payers rarely capture the identifying numbers in electronic health and claims records, citing “administrative burden,” the report said.
The FDA’s “oversight of the safety of medical products, including medical devices” has been “a high-risk issue area” since 2009, the auditors noted.
According to Madris Kinard, a former FDA public health analyst and medical device surveillance expert, the “active surveillance program was supposed to be well under-way by now,” but the GAO report showed that the public health agency has made little progress with the use of the device identifier to monitor the outcome of surgical procedures.
“There are some hospitals using it for some types of implants like heart valves, but it’s not collected for implanted surgical staples and surgical mesh,” said Kinard, who founded Device Events, a firm that analyzes FDA incident data to help patients and doctors track risky medical devices.
“Even though these are relatively inexpensive devices, when something goes wrong it can mean that the patient needs multiple follow-on surgeries, making them high-cost devices in the long term.”
Improper use of identifiers also makes it more difficult for hospitals to identify fraud and protect patients who need to have a recalled or malfunctioning implant removed, Kinard said.
Vaginal mesh was one of around a dozen devices that featured prominently in the Implant Files, a global investigation by ICIJ. The 2018 investigation found that many medical devices later blamed for high numbers of injuries and even deaths, including mesh, were approved in the U.S. without first undergoing clinical trials.
An ICIJ analysis of FDA data cited in the GAO report found that, between 2008 and 2017, more than 1.7 million injuries and nearly 83,000 deaths were potentially linked to the devices in the U.S.
ICIJ analyzed more than 5.4 million “adverse event” reports filed by device manufacturers, importers and hospitals, as well as lawyers and doctors, sent to the FDA. The reports described cases where devices were suspected to have caused or contributed to serious injury or death, or had experienced a malfunction that would likely lead to harm if it were to recur.
Since Implant Files was published, the number of adverse event reports related to devices has soared. There have been an additional 67,000 deaths and more than 4.6 million serious injuries reported to the health agency, according to FDA data extracted by Kinard’s company, Device Events.
The figure may not capture the total number of device-related adverse events because doctors and manufacturers often fail to report them and, when they do, the information can be unverified and incomplete, ICIJ previously found.
This adverse event reporting system is part of the FDA’s “passive” surveillance program that complements the agency’s “active” program involving analyzing UDI data and other information from electronic health records, billing claims, medical device and disease registries to detect medical device safety issues that may otherwise go unreported, the GAO report said.
Though the FDA plans to expand its active monitoring program to other devices in the coming years, so far it has focused on only two types of medical products: duodenoscopes — lighted tubes used for viewing the small intestine associated with numerous infections — and robotically assisted surgical devices used in gall bladder removal.
There are more than 5,000 manufacturers in the U.S. producing thousands of devices for a variety of uses, from surgical masks to pacemakers and MRI machines, according to a 2017 U.S. government report.
The FDA did not respond to ICIJ’s questions on its surveillance program and the GAO’s recent findings.
One of the challenges described by FDA officials to the GAO auditors is that the health agency “does not have the authority to mandate that providers capture such identifiers in electronic health records at the point of care or use identifiers for billing purposes.”
When something goes wrong it can mean that the patient needs multiple follow-on surgeries, making them high-cost devices in the long term.
— Madris Kinard, a former FDA public health analyst and medical device surveillance expert
The GAO report also noted difficulties in obtaining government funding to establish and maintain the active post-market surveillance system, which would cost an estimated $8 million per year.
The FDA requested an increase of $3 million in its fiscal year 2024 appropriation but it did not receive it. In 2022, the agency also proposed using some of the fees it collects from manufacturers to fund its post-market surveillance activities even though the user fees, by law, pay for the FDA’s review and surveillance of products before they are placed on the market, but “industry did not agree to this change,” according to the report.
“If more funding is needed for post-market surveillance, that is up to Congress to determine through the appropriations process,” Advamed’s president Scott Whitaker told ICIJ in an emailed statement. “[W]e are proud of our industry’s support and implementation of the Unique Device Identification program and encourage other stakeholders to utilize the system.”
Since Implant Files, former sales representatives who worked for some device giants have alleged that some manufacturers fail to report their products’ malfunctions to avoid responsibility, and more media reports have emerged exposing injuries and deaths associated with flawed devices.
The congressional watchdog said it “will continue to monitor FDA’s progress in establishing an active postmarket surveillance system.”