After her third child was born, Amanda Dykeman decided to get implanted with Essure, small metal coils placed into the fallopian tubes to prevent conception.
Dykeman, 36, of Orion, Illinois, said her doctor told her the only health risk from the birth control device was the procedure itself. At the time she had the operation in 2010, there was little public information indicating that Essure could fail and harm patients.
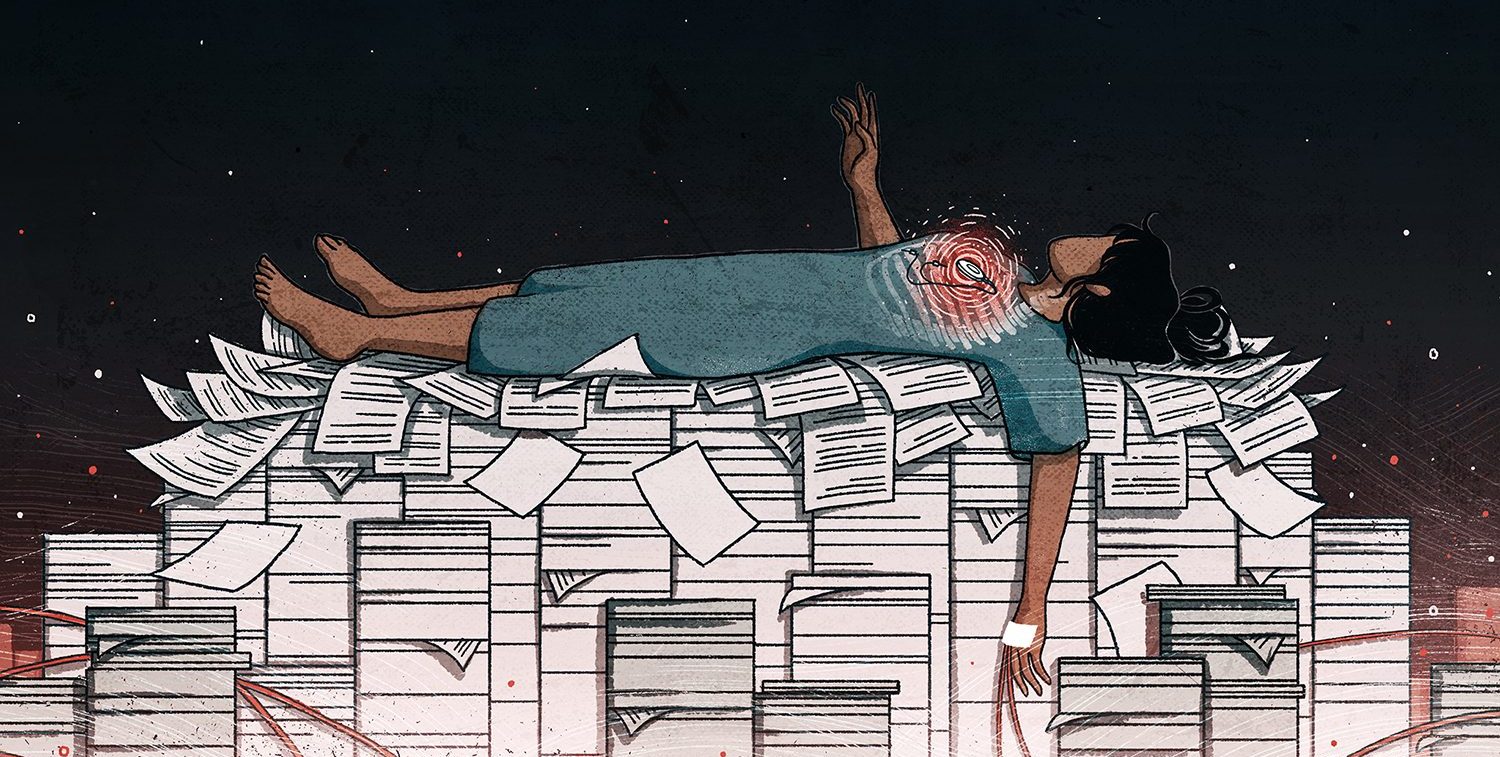
But months after her implant, disturbing symptoms emerged. Dykeman suffered searing pelvic and back pain, extreme fatigue and heavy periods full of blood clots, she recalled in an interview.
“I felt like I had been run over by a Mack truck,” she said.
In 2011, as Dykeman’s ordeal continued, the U.S. Food and Drug Administration discovered that more than 16,000 complaints related to Essure had poured into the device’s manufacturer, Conceptus Inc., between January 2008 and December 2010. But in the same period Conceptus (which has since been acquired by Bayer AG) filed only 182 reports of patient harm with the FDA, the agency found.
Transparency all around would have saved me from getting Essure – Amanda Dykeman
It was not until years later that Dykeman saw the evidence that thousands of other women had suffered problems with Essure. Reports to the FDA of suspected injuries linked to Essure shot from 25 in 2010 to 1,788 in 2014 and 12,564 in 2017, according to FDA data analyzed by the International Consortium of Investigative Journalists for its global Implant Files investigation. Growing concerns about Essure’s safety prompted the FDA to impose a warning of potentially serious or life-threatening risks in 2016 and a sales restriction in 2018.
Bayer announced in July that it will withdraw Essure from the U.S. market at the end of the year, removing it from the last country in the world where it is still sold. Bayer said that the decision was prompted by declining sales and that it continued “to stand behind the product’s safety and efficacy.”
In written responses to ICIJ questions, Bayer said it had complied with FDA rules and that most of the complaints identified in the FDA’s 2011 inspection did not have to be reported under the agency’s guidelines. It also emphasized the limits of adverse events reporting, which the FDA says should not be used in isolation to draw conclusions about whether a device is safe. “We view any unbalanced reporting on adverse events as misleading to the public and potentially dangerous to patients,” said Bayer’s head of communications, Steven Immergut.
The Essure case shows the vital role that reporting of patient harm can play in informing the FDA and other regulators when a device is putting patients at risk — and the extent to which the system for tracking device safety can hide signs of danger from public view, sometimes for years.
“Transparency all around would have saved me from getting Essure,” Dykeman said.
Three failures lead to underreporting of harm
ICIJ’s Implant Files, an investigation into the global medical device industry and its regulators, has identified three critical failures that lead to underreporting of patient harm from implanted devices of all kinds. From public records requests and exclusive data analysis, ICIJ discovered:
- Widespread violations of FDA reporting rules. FDA inspections have found more than 4,400 violations by device companies of its rules for handling complaints and reporting device problems in the last decade. Each violation can include hundreds or even thousands of mishandled complaints.
- Repeated classification of patient deaths as less serious incidents. Manufacturers and others required to report adverse events have classified more than 2,200 episodes in which patients died not as deaths but as injuries, malfunctions or other less severe events in the last five years.
- Burying patient injuries in reports that are not publicly disclosed. The FDA has allowed companies to obscure thousands of injury reports using a program called alternative summary reporting that allows them to keep the information from the public.
The vast majority of FDA incident reports come from manufacturers, which are required by law to report any deaths, injuries or dangerous malfunctions that they suspect may be linked to their products. These reports are made public in a database the FDA calls the Manufacturer and User Facility Device Experience, known as MAUDE.
Across all devices, more than 1.7 million suspected injuries and nearly 83,000 suspected deaths have been reported to the FDA in the past decade, according to an ICIJ analysis.
AdvaMed, the largest trade group for U.S. device manufacturers, disputed the idea that device makers fail to properly report patient harm.
“Companies are extremely cautious about their reporting, often reporting far beyond what is required by regulations,” said Janet Trunzo, AdvaMed’s Head of Technology & Regulatory Affairs. “Any suggestion that manufacturers under-report or somehow mischaracterize their adverse event reports is just wrong.”
The FDA told ICIJ that it has long acknowledged that its system for tracking the safety of devices after they are implanted has “limitations in promptly and consistently identifying safety risks,” and that it is implementing a more proactive “national surveillance system” that will rely on new and existing programs. One initiative, called the National Evaluation System for Health Technology, will use large data sets from electronic medical records and other sources to evaluate device performance. Another, the agency’s relatively new Unique Device Identification System, already requires a unique identifier on the label and package of each device, which among other things is intended to more rapidly track down devices associated with adverse events.
Days before ICIJ began publishing the Implant Files, the FDA announced a goal of being “consistently first among the world’s regulatory agencies to identify and act upon safety signals related to medical devices,” citing the two new programs and others.
With all the shortcomings of its current system, the U.S. does collect and disclose data on adverse events. In most of the world, information on problems that emerge after a device is on the market is either hidden from public view or simply doesn’t exist. Europe’s Eudamed adverse events database remains accessible only to regulators and industry, not the public, and most European countries require Freedom of Information requests to access adverse event reports.
Other countries don’t track medical device problems at all. In Chile, health authorities told ICIJ journalists that adverse event reporting was voluntary for implanted devices and said that they had received only four “relevant” reports in a decade. In Mexico, authorities don’t share adverse event data with the public.
Disagreement on handling complaints
Where there is a process, the first step is a complaint of something gone wrong, often reported to a manufacturer by a patient or doctor.
Some device companies have regularly violated the FDA’s rules for handling these complaints, including discarding many complaints without an investigation, FDA inspectors have found. Other companies abide by the letter of FDA rules but still report only a fraction of incidents linked to their devices, excluding whole categories of incidents as falling outside the scope of their obligations.
In the case of Essure, the FDA found in a 2011 inspection of the company’s headquarters that Conceptus was not informing the agency of complaints of various events including migration of the device within the body and perforation of organs.
“The consensus of the firm management was that if the patient… was asymptomatic then the complaint did not have to be reported,” wrote the FDA inspector.
Bayer said Conceptus had “acted appropriately” and that many of the complaints cited in the inspection did not result in harm to patients or were related to other medical equipment involved in the implant procedure, making them exempt from FDA reporting requirements. Bayer noted that after Conceptus agreed to report certain complaints, the 2011 inspection was eventually closed by the FDA with the agency taking no further action against the company.
Yet in a statement to ICIJ, the FDA said that it requires all episodes of migration of the Essure device to be reported.
“Bayer has been and continues to be required to file MDRs [medical device reports] for incidents of device migration,” said FDA spokeswoman Alison Hunt.
The FDA said that it notified Conceptus that its reporting practices had violated agency guidelines at the conclusion of the 2011 inspection, and that a re-inspection in 2013 found that the company had corrected its problems and was reporting complaints properly.
The FDA also inspects sites abroad belonging to companies that manufacture devices for sale in the U.S., and the agency repeatedly found that they weren’t handling complaints adequately.
Among the violations it identified was a French manufacturer of bone void fillers that had no system for determining whether complaints should be reported to the FDA.
Downgrading deaths
Manufacturers have classified many reports of suspected product-linked deaths as less serious events, an ICIJ analysis of FDA data found. (Read about our methodology, which included the use of machine learning algorithms to screen millions of records.)
In the last five years, manufacturers have designated 220 cases in which patients died as less severe events despite reports that showed that the device may have caused or contributed to the death. In another 1,889 cases, companies downgraded cases of deaths when their own reports did not provide enough information to determine whether the device played a role.
FDA guidelines call on manufacturers to report events that “reasonably suggest” their devices may have caused or contributed to a death, even if the connection is uncertain. Only if there is no suspected association between the device and the death, or if an investigation clears the device, is a company permitted to select a less serious category of event or not report it at all.
But the language of the FDA’s instructions is vague and its policy of allowing manufacturers to decide which incidents to report creates uncertainty, according to Madris Tomes, a former FDA data analyst and the founder of Device Events, a company that tracks medical device adverse events.
“The strict definition of how to report a death is not well written, so it has been manipulated,” Tomes said.
In March 2014, the manufacturer Thoratec Corp. (since acquired by Abbott Laboratories) reported the death of a patient implanted with the HeartMate II, a device that provides mechanical circulatory support to patients with advanced heart disease.
Two suspected causes of death were reported: “suspected pump thrombus,” a device failure in which a blood clot blocks the pump, and multisystem organ failure. Thoratec’s report, which clearly stated that the patient died, designated the incident not as death but as an injury. A follow-up report from the company noted further signs of pump thrombus while describing multisystem organ failure as the primary cause of death.
Pump blockages were a common enough problem among HeartMate II patients that the FDA issued a safety warning about them in 2015. Thoratec and its parent company, Abbott Laboratories, did not respond to repeated telephone and email inquiries from ICIJ.
Trunzo, the regulatory affairs director from AdvaMed, said that reports are based on investigations by companies that rely on multiple sources of information and evolve over time, making it difficult to draw conclusions about whether a device contributed to a death.
“Unless you have access to the company data, patient and hospital information, and unless you trace the incident investigation over time, it is easy to misunderstand the role of the device in a specific incident,” Trunzo said.
Nonetheless, downgrading the severity of reports of suspected patient deaths has significant consequences. FDA analysts review reports in order of priority, starting with deaths, while less serious incidents go to the back of the line. More than half of incoming reports, most of them categorized as malfunctions, do not get read within 60 days, a 2009 report by the Department of Health and Human Services’ Office of the Inspector General found.
The FDA told ICIJ that in 2016 it had updated its guidance to manufacturers on adverse event reporting rules to provide greater clarity.
Michael Drues, a consultant on medical device regulation who advises device manufacturers and regulators, including the FDA and Health Canada, suggested improving results by creating separate categories on FDA reporting forms, one indicating whether the patient died and the other whether the device contributed to the event.
“The bigger problem here is the way that the system is designed,” he said. “And that’s where I think the focus should be.”
Public disclosure
Once events are reported to health authorities, governments decide whether to disclose them to the public.
For nearly two decades in the U.S., an FDA program allowed manufacturers to use a summary reporting program in a way that resulted in large numbers of adverse events not being reported to the public at all.
Under this program, manufacturers submit quarterly spreadsheets summarizing reports of common problems for approved devices. FDA rules specify that the summary reports are not supposed to include incidents that are unusual or that require remedial action to protect public health. They go directly to the agency, which doesn’t disseminate them to doctors, patients or other members of the public.
By allowing companies to report the information without making it public, summary reporting could give the impression of a safe device with low rates of adverse events even when large numbers of problems occurred.
For example, for years the FDA allowed breast implant manufacturers to include ruptures and other serious injuries in summary reports that were not disclosed to the public. In 2017, the FDA became concerned about the practice and quietly directed the companies to report these incidents individually. The result? Adverse event reports associated with breast implants surged more than 20-fold in less than two years.
After this surge and the publication of new studies finding an association between silicone breast implants and autoimmune disease, the FDA has agreed to hold a public hearing next year on breast implant safety.
In its written responses to ICIJ questions, the FDA acknowledged that there was a “transparency issue” with summary reporting and that its 2017 rule change means manufacturers must now publicly disclose the numbers of injuries linked to their products.
Despite these problems, in a major change enacted in August the FDA expanded the use of summary reports for malfunctions — device errors in which patients are not harmed — to all devices, including high-risk ones. Previously only low-risk devices were allowed this non-public option.
The policy change means that reports filed with the FDA about malfunctions of high-risk devices, which by definition involve incidents that could result in injury or death if they recurred, will no longer be visible to the public.
Drues, the consultant and compliance expert, likened the move to ease malfunction reporting obligations to relaxing the academic standards for students in troubled schools.
“Instead of trying to teach these kids better, they lowered the minimum passing grade,” Drues said. “In my opinion that is what the FDA is doing here.”
The device industry used its leverage to win this change. Since 2002, the FDA budget has been partly funded by user fees from device manufacturers under terms negotiated every five years. User fees currently cover 35 percent of the agency’s medical device regulatory activities.
The rollback of reporting rules on high-risk devices was part of the agreement between the FDA and device makers for the 2017 renewal of their user fees, according to the FDA’s description of the new rule.
Trunzo of AdvaMed noted that the new summary reporting program only covers specified malfunctions that are known and understood by device companies and the FDA, and that companies still must file individual reports if a new type of problem occurs. The FDA wrote in the published rule establishing the program that it does not believe that the initiative will have an adverse impact on “the content of information” that it receives.
Crippled capacity
The gaps at each stage of the global surveillance system for implanted devices leave regulators with limited capacity to identify problems.
Tomes, the former FDA data analyst, said expanded summary reporting will likely result in more underreporting and misreporting and that less frequent reports could make it harder to spot trends.
“It’s going to slow the ability of analysts to identify serious problems quickly,” Tomes said.
In Europe, a new medical device regulation enacted in 2017 calls for the Eudamed adverse events database to made public in May 2020, but some experts are skeptical that it will be implemented on time.
Until reporting and transparency policies change, doctors and patients will get little information from public surveillance systems when it comes to making decisions about care.
Dykeman, the Essure patient, had the coils removed in a hysterectomy two years after they were implanted. After the operation, she said, her symptoms cleared and she began organizing with other patients to raise awareness about the device’s risks.
She is now vice president of a patients’ advocacy group called ASHES — Advocating Safety in Healthcare, E-Sisters — that calls for stricter oversight of medical devices.
ASHES helped persuade the FDA to restrict sales of Essure. Dykeman said that better disclosure of device safety problems would help to address the unequal access to information that led to many women’s suffering with the device.
“My mind always just goes back to transparency,” Dykeman said. “I’d like to track the medical devices and put the patients in charge of their own fate.”